At the American Case Management Association (ACMA) 2025 National Conference in Denver, one theme stood out loud and clear: collaboration is everything. Whether partnering with vendors, aligning across health systems, or optimizing internally, the message was consistent—great case management doesn’t happen in silos.
Here’s how collaboration showed up as a key enabler across three areas of healthcare delivery.
Collaboration with Vendors: More Than a Transactional Relationship
Collaboration with vendors should feel like an extension of your care team, not just a contract. When case management leaders strategically leverage vendor relationships, the result is faster workflows and better experiences for patients and staff alike.
Select Tech Vendors Who Collaborate, Not Just Supply
As health systems increasingly rely on technology to streamline referrals and discharge planning, choosing the right tech vendor becomes critical. At this year’s ACMA National Conference, WellSky and Tufts Medicine highlighted how evaluating your current tech stack and selecting the right vendor can transform discharge planning and referral processes, helping to reduce delays and improve care transitions. To ensure seamless integration and collaboration, consider these key factors when selecting a tech vendor:
- Engage the whole referral ecosystem: Onboarding post-acute providers to electronic referral systems is essential for continuity.
- It’s not just about the software: The vendor’s service model, responsiveness, and support are just as critical as platform capabilities.
- Efficiency drives adoption: Reducing clicks, streamlining workflows, and minimizing IT burdens creates real-time value.
- End-user input is crucial: When the people using the tool help select it, adoption and satisfaction soar.
Incorporating vendors that collaborate across systems and care teams helps eliminate silos and ensures smoother transitions between services. The right vendor won’t just provide software—they’ll become an extension of your team, offering continuous support, insights, and an adaptive approach to meet evolving needs.
Use Technology to Build Transparent, Collaborative NEMT Partnerships
When Memorial Hermann relied on a single transportation vendor, delays and inconsistent communication started to impact patient care. Staff had no way to track rides in real time, and all performance data came from the vendor itself—offering little visibility and no accountability.
At the 2025 ACMA National Conference, Memorial Hermann shared how they addressed this challenge by adopting a multi-vendor transportation model supported by Roundtrip. The platform centralized ride booking and surfaced real-time ETAs based on logic set by the health system—not by any one vendor.
- Improved transparency: Staff could see vendor response times, track ride status, and verify performance from a single source of truth.
- Built vendor accountability: Real-time data allowed the system to identify top performers and address issues early.
- Restored trust: Staff gained confidence in the process, and patients experienced more reliable transportation.
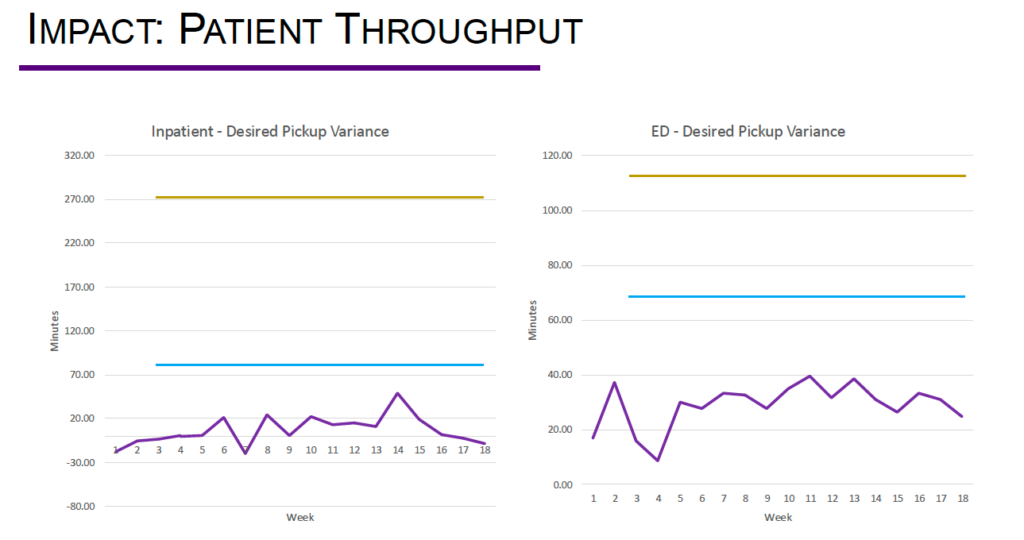
Collaborative vendor networks have immediate impact. Here’s a comparison of single-vendor reported ETAs (blue) and the actual pick-up times (yellow), and how much faster patients were being discharged when leveraging a multi-vendor network through Roundtrip (purple).
Technology turned transportation coordination into a fair, data-driven process—helping Memorial Hermann move from a dependent vendor relationship to a collaborative network. This new infrastructure made it easier to manage vendor relationships fairly. With shared expectations and transparent metrics, high-performing partners could be recognized, while persistent issues could be addressed before they escalated. Staff regained confidence in the system, and patients benefited from more reliable transportation.
Regional Collaboration: Learn from Your Neighbors
Working together across organizations isn’t easy—but when done right, it has the power to improve care for entire communities. Regional collaboration turns individual efforts into collective impact, especially when teams align on data, goals, and communication.
A Northern California Case Study in Regional Collaboration
One session at the conference highlighted how three health systems in the San Francisco Bay Area are setting the bar for cross-organizational collaboration. UCSF Health, Stanford Health Care, and El Camino Health are working together to:
- Share best practices: Improve systemwide performance by implementing strategies that have already been pressure-tested.
- Track high-risk patients: Ensure safe, coordinated transitions across institutions and systems.
- Use collective data: A larger data source can help teams advocate with payers and align incentives.
The power of this model lies in its structure: regular communication, agreed-upon metrics, and a willingness to standardize processes when it benefits the greater good. By aligning on shared goals and using collective data, these health systems are not just improving individual patient journeys—they’re lifting performance across the entire continuum of care.
Strengthen Regional Collaboration Through Your Local ACMA Chapter
One of the most powerful ways to foster cross-organizational connection is by joining your local American Case Management Association chapter. ACMA membership offers a built-in network of peers within your local or regional area, creating space to exchange ideas, align on challenges, and elevate patient care.
Membership gives you access to periodic educational events and an annual chapter conference, where national-level speakers bring fresh insights to your region. Whether you’re sharing best practices or tackling systemic issues, local chapters make it easier to collaborate across institutions.
Internal Collaboration: Driving Organizational Efficiency with Scalable Infrastructure
Collaboration within an organization is just as powerful as partnerships outside of it. At this year’s ACMA National Conference, Northwell Health showcased how internal alignment can transform the case management model across a complex, multi-hospital system.
Centralized Teams, Coordinated Care
When Northwell Health saw that delays in post-acute authorizations were increasing length of stay and pulling clinical staff away from patient care, they knew a centralized, collaborative approach was needed. By creating a dedicated administrative team to manage authorizations and transportation across hospitals and medical centers, they streamlined operations and freed up clinicians—leading to:
- Reduced turnaround time: Authorization times dropped by nearly half a day.
- Improved clinical focus: With less administrative burden, clinical staff spent more time on top-of-license care.
- Enhanced satisfaction: Patients and employees reported better experiences, thanks to smoother transitions and clearer communication.
Although this new infrastructure drove change, the key to its success was alignment. Open communication ensured every stakeholder understood the ‘why’ behind the changes. Shared workflows created consistency across teams and locations, making handoffs smoother and reducing variability. Performance measurement tied it all together, allowing leaders to track progress, identify gaps, and continuously refine processes. By aligning people, processes, and data, Northwell Health turned administrative coordination into a strategic asset.

Enterprise Care Models Build Across Systems
When care coordination isn’t streamlined across systems, it can lead to inefficiencies that hinder patient outcomes, drive up readmissions, and prevent effective throughput. To address this, Northwell Health developed a corporate care coordination model aimed at enterprise-wide performance standards and quality improvement across multiple hospitals.
- Built a Corporate Care Coordination team to support throughput, readmission reduction, and denial prevention.
- Standardized onboarding, training, and competencies with a dedicated education team and robust reporting structure.
- Leveraged data and dashboards to give leaders real-time insights into utilization review, productivity, and care transitions.
- Aligned EMR workflows with best practices, embedding care coordination into every phase of the patient journey.
These efforts represent a clear shift toward top-of-license practice, centralized strategic alignment, and scalable improvement. By building collaboration into their care models, Northwell showed that internal coordination isn’t just operationally effective—it’s essential to delivering patient-centered care.
Collaboration Isn’t a Buzzword—It’s a Strategy For Better Case Management
Collaboration, from vendor partnerships to regional alliances to internal systems, is essential for modern case management. It enhances efficiency, boosts patient outcomes, and empowers teams to perform at their best. The challenge lies in creating those connections deliberately. The reward is a unified care system that functions seamlessly.
The most important thing about collaboration? You can’t do it alone. Whether you’re working to coordinate transportation across vendors, align ride booking across your health system, or bring more consistency to your tech and workflows, Roundtrip can help. Talk to us to learn how we support smarter, more connected care.
